AORTA
The aorta is the main artery from which all organs in the body receive their arterial blood supply. Arterial blood contains oxygen and other nutrients. This is delivered to the various organs by means of the heart that pumps blood through the arteries to the organs.
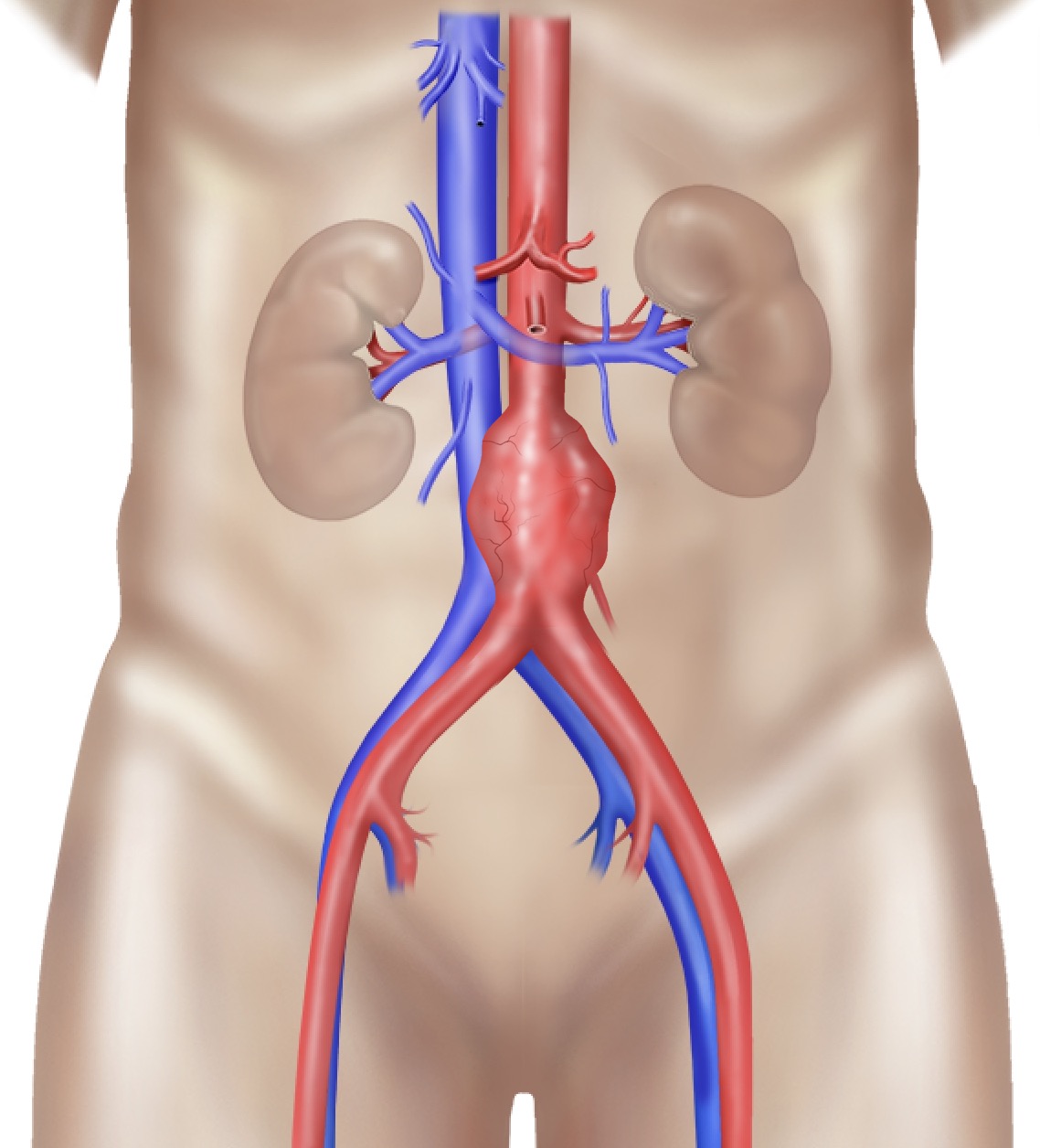
The aorta is the largest artery in your body and it carries blood away from your heart. Your aorta runs through your chest, where it is called the thoracic aorta. When it reaches your abdomen, it is called the abdominal aorta. The abdominal aorta supplies blood to the lower part of the body. Just below the abdomen, the aorta splits into two branches that carry blood into each leg.
Abdominal aortic aneurysm
When a weak area of the abdominal aorta expands or bulges, it is called an abdominal aortic aneurysm (AAA). The pressure from blood flowing through your abdominal aorta can cause a weakened part of the aorta to bulge, much like a balloon. A normal aorta is about 16 to 18 mm in diameter. However, an AAA can stretch the aorta beyond its safety margin (> 55mm). Aneurysms are a health risk because they can burst, or rupture. A ruptured aneurysm can cause severe internal bleeding, which can lead to shock and even death.
An aneurysm can cause another serious health problem: blood clots or debris can form inside the aneurysm and travel to blood vessels leading to other structures in your body. If one of these blood vessels becomes blocked, it can cause severe pain or even limb loss.
Each year, physicians diagnose approximately 200 000 people in the United States with AAA. Of those 200 000, nearly 15 000 may have AAA threatening enough to cause death from a ruptured aneurysm if not treated.
Fortunately, when diagnosed early, AAA can be treated, or even cured, with highly effective and safe treatments.
Symptoms
Although you may not feel any symptoms with AAA, if you develop symptoms, you may experience one or more of the following:
A pulsing feeling in your abdomen, similar to a heartbeat above your belly button
Severe, sudden pain in your abdomen or lower back. If this is the case, your aneurysm may be about to burst
If your aneurysm bursts, you may suddenly feel intense weakness, dizziness, or pain and you may lose consciousness. This is a life-threatening situation and you should seek medical attention immediately
Causes
hysicians and researchers are not quite sure what causes AAA. The leading thought is that the aneurysm may be caused by inflammation in the aorta, which may cause its wall to break down. Some researchers believe that this inflammation can be associated with atherosclerosis (also called hardening of the arteries) or risk factors that contribute to atherosclerosis, such as high blood pressure (hypertension). In atherosclerosis fatty deposits, called plaque, build up in an artery. Over time, this buildup causes the artery to narrow, stiffen and possibly weaken. Besides atherosclerosis, other factors that can increase your risk of AAA include:
Age: Being older than 60 years
Genetics: Immediate relative who has had AAA
High blood pressure (hypertension)
Smoking
Gender: AAA is more common in men than in women
Tests
Abdominal aortic aneurysms can be palpated during clinical examination. They are most often found when a physician is performing an imaging test, such as an ultrasound, for another condition. If your physician suspects that you may have AAA, he or she may recommend one of the following tests:
Abdominal ultrasound
Computed tomography (CT) scan
Magnetic resonance imaging (MRI)
Treatment Options
Watchful Waiting
Your physician may recommend "watchful waiting," which means that you will be monitored every 6 months for signs of changes in the aneurysm size. Your physician may schedule you for regular CT scans or ultrasound examinations to watch the aneurysm. This method is usually used for aneurysms that are smaller than 55mm. If you also have high blood pressure, your physician may prescribe blood pressure medication to lower your blood pressure and lower the pressure on the weakened area of the aneurysm.
Surgical Repair
A vascular surgeon may recommend that you have a surgical procedure called an open aneurysm repair if your aneurysm is causing symptoms or is larger than 55mm, or is enlarging rapidly under observation. During an open aneurysm repair, also known as surgical aneurysm repair, your surgeon makes an incision in your abdomen and replaces the weakened part of your aorta with a tube-like graft. This graft is made of man-made material, such as polyester, in the size and shape of the healthy aorta. The tube strengthens your aorta and allows blood to pass easily through it. Following the surgery, you may stay in the hospital for 5 to 7 days. You may also require 2 to 3 months for a complete recovery. More than 95 percent of open aneurysm repair are successful for the long term.
Endovascular Repair
Instead of open aneurysm repair, your vascular surgeon may consider a newer procedure called an endovascular abdominal aortic aneurysm repair with an endovascular stent graft. Endovascular means that the treatment is performed inside your body using long, thin tubes called catheters that are threaded through your blood vessels from the groin. This procedure is less invasive, meaning that your surgeon will make only small incisions in your groin area through which to thread the catheters. During the procedure, your surgeon will use live x-ray pictures on a screen to guide a fabric and metal tube, called a stent graft, to the site of aneurysm. Like the graft in open surgery, the endovascular stent graft also strengthens the aorta. Your recovery time for endovascular stent graft is much shorter than surgery, and your hospital stay is reduced to 2 to 3 days. However, this procedure is more likely to require periodic maintenance than the open procedure. In addition, you may not be suitable to have this procedure, since not all patients are candidates for endovascular repair. In some cases, open aneurysm repair may be the best way to cure AAA.
Open Surgical Reapir

Endovascular Repair

Aortailiac Occlusive Disease
Some patients develop occlusion of the abdominal aorta and its end branches, named the iliac arteries. Patients often complain of difficulty when walking (claudication). This problem can be resolved by means of a bypass or endovascular procedure.
Aorto-iliac occlusive disease occurs when your iliac arteries become narrowed or blocked. The aorta, your body's main artery, splits into branches at about the level of your belly button. These branches are called the iliac arteries. The iliac arteries go through your pelvis into your legs, where they divide into many smaller arteries that run down to your toes. Aorto-iliac disease is considered a type of peripheral arterial disease (PAD), because it affects arteries that carry blood away from your heart to your limbs.
Your arteries are normally smooth and unobstructed on the inside, but as you age, it becomes hard and irregular due to cholesterol plaque that builds up in the walls of your arteries. Plaque is made up of cholesterol, calcium, and fibrous tissue. As more plaque builds up, it causes your arteries to narrow and stiffen. This process is called atherosclerosis, or hardening of the arteries. Eventually, enough plaque builds up to interfere with blood flow in your iliac arteries or leg arteries. Physicians call this aorto-iliac occlusive disease.
When your iliac arteries narrow or become blocked, your legs may not receive the blood and oxygen they need. This lack of oxygen is called ischaemia and it can cause pain. In severe cases, sores (ulcers) or gangrene can develop, which can result in you losing a limb if not treated. However, these symptoms are uncommon.

Symptoms
Early in the disease, you may feel pain, cramping or fatigue in your lower body when you walk or exercise. The pain with walking usually occurs in your buttocks, thighs, and legs. This symptom is called intermittent claudication because it stops when you rest. The maximum distance that you are able to walk might vary. As the disease worsens, you may find that pain occurs when you walk for shorter distances. (Shortening claudication distance) Ultimately, you may feel pain, usually in your toes or feet, even when you are resting. (Rest pain)
Some men who have aorto-iliac occlusive disease also experience erectile dysfunction, the inability to have or maintain an erection.
Aorto-iliac disease may worsen if it is not treated. Signs that it has advanced include:
Severe pain, coldness, and numbness in a limb
Sores on your toes, heels, or lower legs
Dry, scaly, cracked skin on your foot. Major cracks, or fissures, may become infected if left untreated
Weakened muscles in your legs
Gangrene (tissue death), which may require amputation
If you experience any of these advanced symptoms, it usually means that your leg arteries are blocked in more than one place. Your physician may need to treat more than one site to prevent gangrene or limb loss.
Causes
Atherosclerosis, or hardening of the arteries, causes most cases of aorto-iliac occlusive disease. Risk factors for hardening of the arteries include:
Smoking
High cholesterol
High blood pressure
Obesity
Having a family history of heart disease
In rare cases, a condition known as Takayasu’s arteritis may cause blockages in your aorta and its branches. Takayasu’s arteritis usually affects young women between the ages of 10 and 30.
Tests
First your physician asks you questions about your general health, medical history, and symptoms. In addition, your physician conducts a physical exam. Together these are known as a patient history and exam. As part of your history and exam, your physician will ask you if you smoke or have high blood pressure. Your physician will also want to know when your symptoms occur and how often. A pulse examination that checks your pulse in several places in your legs for weak or absent pulses is part of your physical exam. For this test, your physician will simply place his or her fingers over pulse points
After the history and exam, if your physician suspects you may have aortoiliac disease, he or she will perform tests, such as:
Ankle-brachial Pressure Index (ABPI):
For the ABPI, your physician measures your blood pressure in your ankle and in your arm. Your physician will compare the two numbers to determine your ABPI. Normally, the blood pressures in your ankle is slightly higher than in your arm. But if your ankle pressure is half your arm pressure (or lower), your leg arteries are probably significantly narrowed. To perform the ABPI, your physician will use an ordinary blood pressure cuff and an ultrasound device (handheld Doppler). The ABPI helps your physician diagnose aorto-iliac disease, but it does not identify which arteries are blocked.
Doppler Ultrasound:
Doppler ultrasound (arterial duplex-Doppler) uses high-frequency sound waves that bounce off of blood cells and blood vessels to show blood flow and problems with the structure of blood vessels. This test identifies specific arteries that are blocked.
Angiography:
In this test, your physician injects a contrast dye into your arteries and then takes x-rays. The structure of your arteries appears on the x-ray because x-rays cannot pass through the dye. This test finds the exact location and pattern of blockages.
Treatment Options
Lifestyle Changes
In mild to moderate cases, your physician may recommend that you change certain aspects of your lifestyle. If you are a smoker, the most important step you can take is to quit smoking immediately. Chemicals in tobacco damage your arteries. These chemicals can also increase your chance of having complications from aorto-iliac occlusive disease.
In addition to quitting smoking, your physician may recommend that you maintain a healthy weight, follow a structured walking program at least 3 or 4 times a week, and eat a low-fat and high-fiber diet. These changes help slow hardening of the arteries.
If you have diabetes, you need to control your blood sugar levels. If you have diabetes, your physician may recommend that you receive foot care from a qualified healthcare professional (Podiatrist) and learn the basics of caring for your feet at home. This includes practicing foot hygiene, wearing protective, well fitting and cushioned footwear, and avoiding injuries to your foot. This type of care can be very important because you can lose feeling in your feet and develop sores on them.
Medication
If you do not have a disqualifying medical condition, your physician may also prescribe pentoxifylline, which can improve the distance you are able to walk without pain. Other drugs your physician may prescribe include aspirin or clopidogrel, either of which can lower your chances of blood clots. Cholesterol lowering medication is usually prescribed. Blood pressure and blood glucose must be addressed by optimal medical therapy.
Intervention
If you have severe aorto-iliac occlusive disease, particularly if it does not improve with the measures described above, your physician may recommend surgery or a minimally invasive endovascular treatment called angioplasty to improve the circulation in your legs. The choice of the treatment depends upon the pattern and extent of the blockages.
Intervention:
Angioplasty with or without stent
In an angioplasty, a long, thin, flexible tube called a catheter is inserted into a small puncture over an artery in your leg and is guided through your arteries to the blocked area. Once there, a special balloon attached to the catheter is inflated and deflated. The balloon pushes the plaque in your artery against your artery walls, widening the vessel. A tiny mesh-metal tube called a stent may then be placed into the narrowed area of your artery to keep it open. The stent remains permanently in your artery. After successful angioplasty, blood flows more freely through your artery.
Intervention:
Endarterectomy
An endarterectomy is a way for your surgeon to remove the plaque from your artery. To perform an endarterectomy, your vascular surgeon makes an incision in your leg and removes the plaque contained in the inner lining of the diseased artery. This leaves a wide-open artery and restores blood flow through your leg artery.
Intervention:
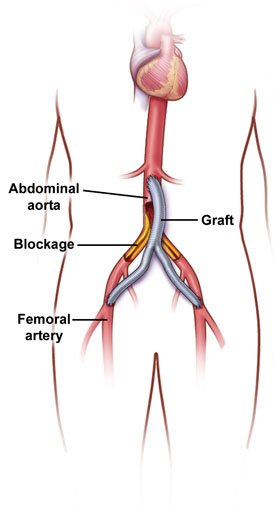
Bypass surgery
Bypass surgery creates a detour around the narrowed or blocked sections of your artery. An inverted Y-shaped tube made of synthetic fabric, called a graft, is attached to your aorta above the blockage. The two branches of the graft are then attached to either your left and right iliac arteries or other major arteries in each leg (called the femoral arteries). Bypass surgery restores blood flow in about 85 percent of patients. Results are commonly maintained for 10 or more years.
Iliac Angioplasty and Stent

Endarterectomy

Aorta-bifemoral Bypass Graft

Our Services
Arterial
Procedures
Standard open arterial surgical procedures to repair aorta aneurysm and / or reconstruct blood flow to the lower extremities.
Open aorta aneurysm repair
Aorta-bifemoral bypass
Iliofemoral bypass
Endarterctomies
Endovascular
Procedures
Less invasive percutaneous procedures to repair blood flow through the aorta to intestines, organs and extremities.
Mesenteric artery angioplasty
Renal artery angioplasty
Aorta angioplasty
Iliac artery angioplasty
Subclavian artery angioplasty
Hybrid
Procedures
Combined endovascular and opens surgical procedures to repair abdominal aorta aneurysms, thoracic aneurysm or to improve blood flow to the extremities.
Endovascular abdominal aorta aneurysm repair
Endovascular throacic aorta aneurysm repair
If you have any problems with any of these conditions, please contact your General Practitioner, or your Vascular Surgeon. If you live in Pretoria and have not seen a Vascular Surgeon before, you are more than welcome to contact my rooms for a formal consultation.
Gregory Weir Vascular Surgery
The purpose of this web site is to offer Dr Weir’s patients and their families access to information regarding vascular disease in general as well as specific information on certain disease processes. The information on this site does not necessarily apply to all patients with the same diagnosis. If you are not a patient of Dr Weir, please do not regard the information on this website as a substitute for a thorough assessment by a qualified Vascular Surgeon. If in doubt, consult your doctor.
If you are experiencing a medical emergency, phone us. If you are not able to get through or if we are not available, please visit your nearest casualty department.
Consultation Rooms
Vascular & Hyperbaric Unit, Life Eugene Marais Hospital, Pretoria